
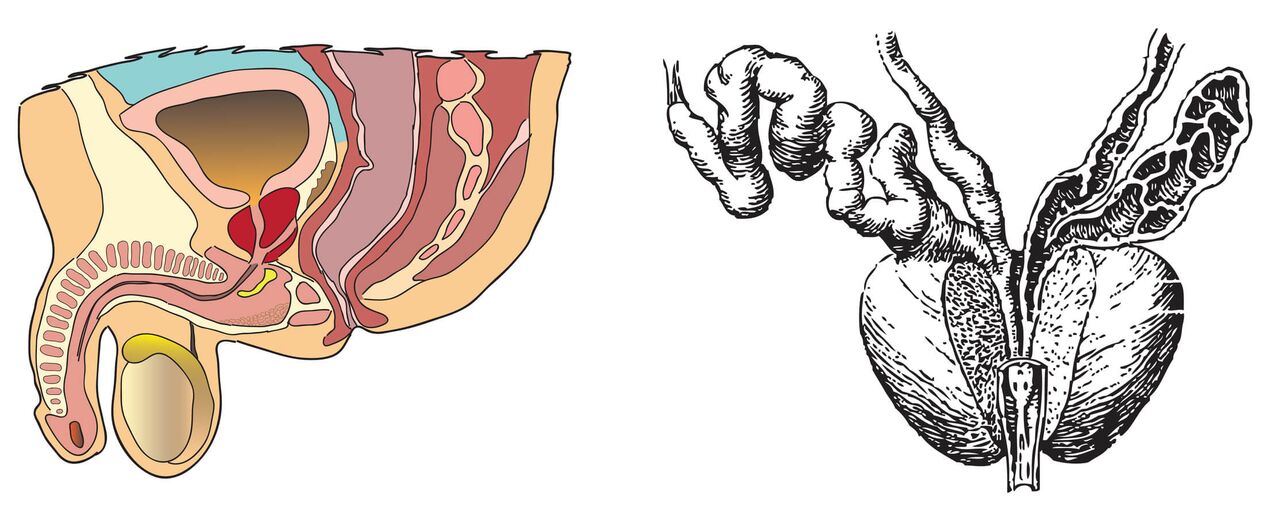
ProstatitisIs a urological disease accompanied by inflammation of the prostate gland tissue. Damage to the prostate can be caused by an infection transmitted through the blood, lymph, or through unprotected sexual intercourse. The development of prostatitis in men is facilitated by injury and disruption of blood supply to the pelvic organs, persistent hypothermia, low physical activity, hormonal imbalances and other factors. Prostatitis can be accompanied by vesiculitis, urethritis and other infectious and inflammatory diseases of the reproductive and urinary organs.
Incident statistics
Prostatitis is one of the most widespread diseases of the male genitourinary system in the world. According to various sources, it is observed in 60-80% of sexually mature men. According to official medical statistics, more than 30% of young people of reproductive age suffer from chronic prostatitis. In about a third of cases, it occurs in men over 20 years of age. According to the WHO, urologists diagnose chronic prostatitis in every tenth patient.
Causes of prostatitis
Infection.Pathogenic and opportunistic bacteria enter the prostate through lymphatic and blood vessels. Secondary prostate infections are often a complication of inflammatory diseases of the rectum and urethra.
Type of infection:
- ascending- microbes rise to the glands from the opening of the external urethra;
- down- microbes enter the prostate along with the infected urine stream.
Conditional pathogenic microorganisms that provoke disease (according to the Urological Research Institute 1997-1999)
| Microorganisms | Number of studies | |
|---|---|---|
| % | abs | |
| Staphylococcus epidermidis | 42. 3 | 55 |
| S. saprophyticus | 17. 6 | 23 |
| S. aureus | 4. 6 | 6 |
| S. haemolyticus | 3. 1 | four |
| S. hominis | 0. 8 | one |
| S. warneri | 1. 5 | 2 |
| Staphylococcus spp. | 3. 1 | four |
| Enterococcus faecalis | 11. 6 | fifteen |
| Streptococcus spp. | 3. 1 | four |
| TOTAL (gr. +) | 87. 6 | 114 |
| P. aeruginosa | 3. 7 | five |
| And coli | 4. 7 | 6 |
| Enterobacter spp. | 2, 3 | 3 |
| Proteus spp. | 1. 5 | 2 |
| TOTAL (gr. -) | 12. 3 | sixteen |
Weakened immunity.One of the causes of prostate inflammation is the weakness of the body’s immune defenses. This can be facilitated by frequent stress, unbalanced diet, overwork, smoking, alcohol intake. With diminished immunity, the body is most susceptible to infections that lead to the development of prostate disease.
Disruption of blood supply.The development of chronic prostatitis can be the result of an inactive and inactive lifestyle. With a constant lack of physical activity, the work of the endocrine, cardiovascular and nervous systems, as well as blood circulation in the pelvic organs is disrupted. The result is oxygen starvation of the prostate tissue.
Irregular sexual activity.Both prolonged sexual abstinence and excessive sexual activity can contribute to the appearance of prostatitis. Many sexually active men experience nervous exhaustion, hormonal imbalances, disrupted sex gland secretions, and a gradual fading potential. Disrupted sexual intercourse has a negative impact on the health of the prostate gland.
Chronic prostate injury. . . Chronic prostatitis can develop as a result of frequent trauma to the soft tissues of the prostate gland. Often this is observed in patients whose professional activities are related to driving. The cause of prostatitis in this case is constant tremors, vibrations and excessive pressure on the perineum muscles.
The main syndrome of prostatitis
It hurts.With prostatitis in men, there is pain and soreness in the lower abdomen and lower back, as well as pain throughout the body. These symptoms can worsen with ejaculation, especially during sexual intercourse after prolonged abstinence.
Dysuria.Special signs of prostatitis in men often urge to urinate, burning and stinging when emptying the bladder, pulling pain after urination in the perineum. Another symptom of prostate inflammation is difficulty urinating. If there is no treatment for the disease, acute urinary retention may occur.
Sexual dysfunction.With uncomplicated prostatitis, there is accelerated ejaculation, wearing of orgastic sensations, pain during ejaculation, partial or total decrease in libido. Prolonged erections at night are also a symptom of chronic prostatitis.
External manifestations.With prostatitis, some patients experience purulent or clear discharge from the urethra, most of which occurs in the morning. Patients may also notice symptoms such as the presence of white flakes or filaments in the urine.
Types of prostatitis
Acute bacteria.Acute prostatitis develops as a result of infection of the prostate gland with Staphylococcus aureus, Escherichia coli, enterococcus and other pathogenic bacteria. If left untreated, the disease can trigger blood poisoning. In this case, the man should be immediately hospitalized.
Symptoms observed with this type of prostatitis:
- chills and fever (38 ° C and above);
- sharp or pulling pain in the groin, lower back and perineum;
- frequent urination;
- painful urination;
- difficulty urinating and acute urinary retention;
- whitish or colorless whiteness of the urethra.
Chronic bacteria.Recurrent forms of the disease occur as a result of the penetration of infection into the glands. Chronic hypothermia, prolonged sexual abstinence, and irregular urination contribute to the development of prostatitis. Chronic prostatitis, if left untreated, can provoke cystitis, because inflammation of the prostate is a storage of bacteria that affects the genitourinary tract.
Symptoms of chronic prostatitis:
- pain in scrotum, lower abdomen, perineum;
- dysuria;
- potential violation.
Not chronic bacteria.Causes of this disease include the entry of viruses or bacteria into the prostate (tubercle bacillus, Trichomonas, chlamydia), autoimmune processes, the penetration of urine into the glands. Chronic prostatitis accounts for up to 95% of all types of prostate inflammation.
The signs of prostatitis are:
- chronic pain in the pelvic area (bothering men for at least 3 months);
- recurrent groin pain;
- absence of inflammatory symptoms in urine, semen and prostate secretions.
Chronic asymptomatic.Asymptomatic chronic prostatitis is not associated with bacterial infection and symptomatic prostate syndrome. There is an assumption that the disease is an age -related physiological feature.
Symptoms of this type of chronic prostatitis:
- the absence of the main syndrome of the disease;
- increased content of leukocytes and bacteria in urine.
The main symptom of this disease - the presence of infection in the gland - can only be detected by biopsy or during surgical operations in the treatment of various pathologies of the prostate (adenoma, cancer).
Blocked.Prostatitis develops not only against the background of anatomical and physiological changes in the venous system and other bodies. The main cause of this disease is an irregular sex life.
Signs of prostatitis:
- pain in the perineum, radiating to the sacrum;
- increased urination in the morning;
- slight difficulty in the outflow of urine (symptoms are observed in the form of chronic diseases);
- erectile dysfunction;
- decreased libido;
- "Pale" sensation of orgasm during ejaculation.
Diagnostics of acute and chronic prostatitis
To choose the right method of treatment, the doctor prescribes a comprehensive diagnosis of the state of the genitourinary system, including the following methods.
Digital rectal examination.If you suspect prostatitis, a urologist performs a digital examination. The posterior surface of the prostate is close to the rectum, so when a finger is inserted through the anus, the doctor can determine the condition of the gland. In this study, its size, consistency and shape, surface condition, pain were determined.
Signs of prostatitis in men include:
- soft and inelastic consistency of the prostate;
- pain on palpation;
- enlarged glands;
- immobility of the rectal mucosa over the prostate.
Ultrasound procedure.Prostate ultrasound is prescribed before the start of treatment for acute prostatitis to identify / exclude glandular abscesses, and in the chronic process of the disease - to identify cysts and prostate stones, as well as the degree of urethral compression. The most effective method is rectal ultrasound.
Uroflowmetry.This method of diagnosis of prostatitis is used to study the indicators of the process of urination: the duration of this physiological action and the rate of urine outflow. If the velocity is 15 ml / s or more, this indicates a normal state of the urethra. A sign of prostatitis is a decrease in this value below 10 ml / s. This speed is due to the lack of urinary tract patents.
Interpretation of uroflowmetry results
| Urine flow rate | Interpretation |
|---|---|
| >15ml / sec | Urinary tract obstruction is unlikely to occur |
| <10ml / sec | Possible urethral narrowing or detrusor weakness may occur |
| 10-15ml / sec | The results are uncertain |
Cystoscopy.For examination, an endoscopic imaging system is inserted into the bladder. Methods for diagnosing acute and chronic prostatitis are used when diseases such as cancer, cystitis, or trauma to the bladder are suspected.
Laboratory research.To diagnose and determine the microorganisms that cause the disease, in the presence of symptoms of chronic prostatitis or acute inflammation, urine and prostate secretions are examined. A sign of the presence of pathogenic microflora is an increase in the number of leukocytes in the biological material. To devise an effective treatment method, bacterial types were determined by PCR, RIF and inoculation on nutrient medium.
Interpretation of laboratory results
| Prostate secretions | Third urine sample (after prostate massage) | |||
|---|---|---|---|---|
| HP Form | Number of leukocytes, uv. x 400 | Sowing results | Number of leukocytes, uv. x 400 | Sowing results |
| Bacteria | >10 | + | The difference between the number of leukocytes in the third part of the urine and the second part of the urine is ≥10 | + |
| Chronic pelvic pain inflammatory syndrome | >10 | - | The difference between the number of leukocytes in the third part of the urine and the second part of the urine is ≥10 | - |
| Chronic non -inflammatory pelvic pain syndrome | <10 | - | - | - |
Prevention of prostatitis

Physical activity.For the prevention and treatment of prostate disease, a man must avoid physical activity. Recommended:
- walking (4 km a day or more);
- exercises (squats, jumps, bends);
- perineum and back muscle exercises (10 tension and relaxation).
Proper nutrition.For the prevention of acute and chronic prostatitis, men should include in their diet foods high in zinc and vitamin B. It is recommended to eat:
- seafood (oysters, seaweed);
- meat;
- pumpkin seeds;
- walnut;
- bran;
- kefir;
- Bread bread.
Frequent sex life.While preventing and treating disease, a man needs:
- living a rhythmic sex life;
- avoid interrupted sexual intercourse;
- avoid casual relationships.
Treatment of acute and chronic prostatitis
Prostate inflammation is treated using the following methods.
Antibacterial therapy.If prostatitis is bacterial, antibiotics are needed to treat it. Doctors choose a group of drugs depending on the type of microbe that causes the disease, the sensitivity of the pathogen to various drugs, and the presence of contraindications in the patient.
Drug properties
| Medicine | Benefit | ugliness |
|---|---|---|
| Fluoroquinolones |
|
|
| Macrolide |
|
Not active enough against gram -negative bacteria |
| Tetracyclines | Active against atypical pathogens |
|
Hormone therapy.Hormone treatment is needed to restore the normal hormonal balance between androgens and estrogens. Drugs with antiandrogenic activity reduce inflammation of glandular tissue and prevent the transition of the disease to a more severe stage.
Prostate massage.This method of treating chronic prostatitis can only be used outside of exacerbations. A man should take a prone position, place his palms on the couch or table, spread his legs shoulder -width apart. The doctor performing the treatment wears sterile gloves on his hands, applies an ointment or gel (in some cases, a drug with an anesthetic component) to the index finger of his right hand, and injects it through the anus into the rectum. The massage is performed by applying a little pressure until the prostate secretions are separated through the opening of the urethra. The treatment involves at least 10 massage sessions.
Physiotherapy.To treat the symptoms of prostatitis, methods are used to normalize and improve blood circulation in the pelvic area. This allows you to exclude stagnation, as well as increase the effectiveness of drug therapy. Treatment is performed by exposing the gland to ultrasonic waves, electromagnetic vibrations, as well as high temperatures (microclycer with warm water).
Surgical intervention.Surgical intervention for prostate disease is rarely used. Such treatment is mandatory for the development of complications of acute or chronic prostatitis.
Indications for prostate surgery:
- acute urinary retention due to severe urethral narrowing;
- abscess (appearance of suppuration on the surface of the gland);
- glandular sclerosis;
- adenomas that do not respond to conservative treatment.
Complications of prostatitis

Vesiculitis.Untreated prostatitis can cause inflammation of the seminal vesicles. Symptoms of the disease are pain in the pelvis, radiating to the sacrum, exacerbated by erection and ejaculation, frequent urination, the appearance of blood and / or pus in semen and urine.
Coliculitis and urethritis.Due to its proximity to the excretory flow of the prostate, the seminal tubercle is often inflamed as a result of infection from an infected gland. If left untreated, the symptoms of prostatitis are complemented by the special symptoms of urethritis - burning or tingling in the urethra when urinating. There is also pain during ejaculation due to a spasmodic urethral contraction.
Prostate abscess.The appearance of purulent cavities on the surface of the gland is caused by pathogenic bacteria that cause prostatitis. Special symptoms of the disease are general weakness, impaired consciousness, confusion, sharp rise in temperature, increased sweating, chills. Prostate abscess is a severe septic disease that must be treated in a hospital setting.
Prostate sclerosis. Prostate sclerosis develops against the background of exacerbation of chronic prostatitis due to non -adherence to treatment prescribed by urologists. The disease can form over several years, however, if the hormonal balance in the male body is disturbed, its rapid development is possible. With prostate sclerosis, pain is observed during emptying of the bladder, intermittent and slow flow of urine.
Formation of cysts and stones. . . The appearance of cysts in the gland is one of the possible options for the development of chronic prostatitis. Infection with neoplasms can cause abscesses and greatly complicate the treatment of the disease. Single and multiple stones can also form in the prostate. In this disease, in addition to the usual symptoms of chronic prostatitis, there is a violation of the outflow of urine, frequent urination, pain in the perineum.
Infertility.In chronic prostatitis, sperm production and motor function are impaired. If left untreated, the disease also affects the vas deferens and seminal vesicles, making them unable to release sperm, so that they are not thrown into the urethra during ejaculation. As a result, men with chronic prostatitis often experience infertility.



























